| Royal City Drugs |
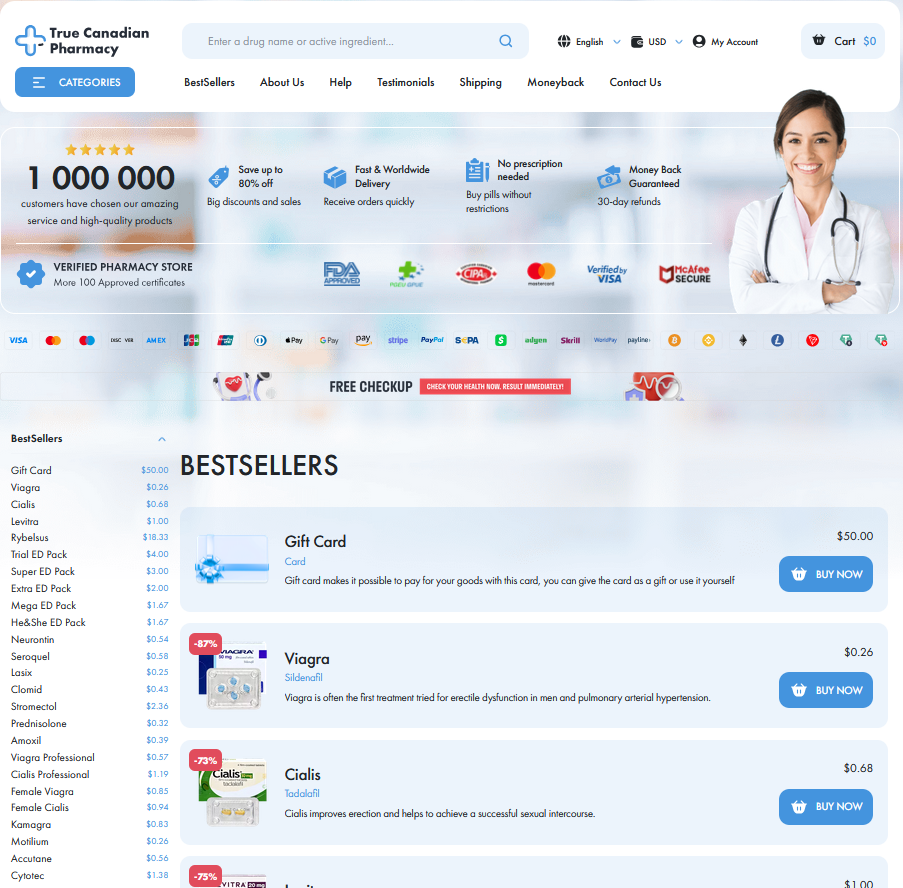
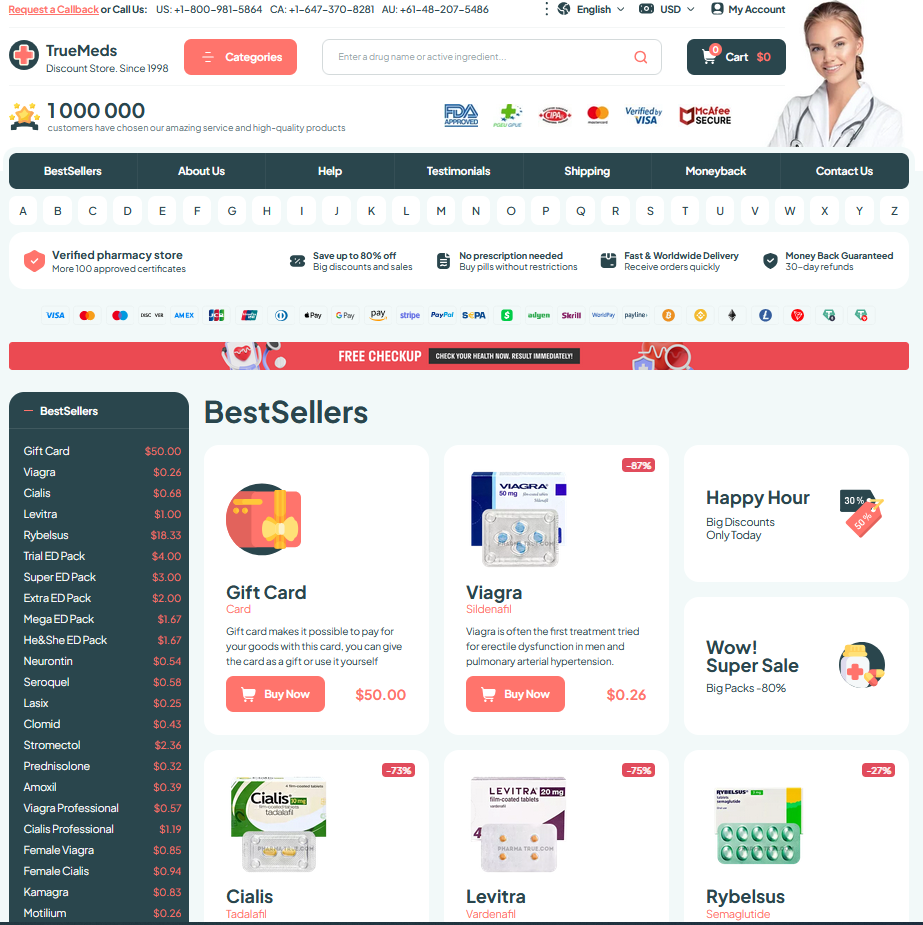
To Visit Online Pharmacy Click HERE ↓
Bactrim Resistance: Causes and Prevention Strategies
How Bacteria Outsmart Trimethoprim-sulfamethoxazole: Core Mechanisms
Bacteria are small storytellers, adapting quickly when exposed to trimethoprim-sulfamethoxazole. The duel is microscopic but consequences are immense for patients.
They change drug targets, pump out medicines, or grab resistance genes from neighbors. Enzymes inactivate drugs and often bypass blocked pathways.
Mutations tweak enzyme shapes so the drugs no longer bind, while efflux pumps lower doses. Biofilms and slow growth create refuges, Wich protects subpopulations from exposure.
Mobile genetic elements such as plasmids spread traits across species, creating pockets of untreatable infections; surveillance and smarter prescribing can slow this tide.
Common Clinical Causes Driving Antibiotic Resistance Emergence

Clinicians often confront a familiar scene: a patient returns days after starting therapy, symptoms unchanged and cultures showing resistance. Teh routine drivers are predictable—incomplete courses, subtherapeutic dosing, and empiric broad‑spectrum therapy that applies intense selection pressure. Frequent prophylactic use, especially in chronic conditions, and repeated cycles of antibiotics like bactrim create ecological niches where resistant strains flourish, turning short-term fixes into long-term hospital and community problems.
Diagnostic delays and failure to tailor therapy to susceptibility profiles amplify selection: when labs arent timely, clinicians continue ineffective regimens and resistant clones gain footholds. Device-associated infections, biofilm formation, and immunosuppressed hosts provide refuges where resistant bacteria silently multiply. Gaps in infection control, overcrowding, and poor antibiotic access that encourages partial courses further compound the problem. Recognizing these clinical patterns allows targeted interventions—rapid diagnostics, dose optimization, and rigorous infection control can interrupt resistance trajectories.
Role of Misuse and Overprescription in Resistance Spread
Clinicians and patients tell stories of quick fixes: a cough, a sore throat, and a prescription for bactrim handed out like candy. When antibiotics are used for viral illnesses or stopped early, selective pressure lets resistant strains flourish, turning simple infections into stubborn, dangerous problems. These narratives hide systemic drivers — diagnostic uncertainty, patient demand, and time-pressed clinics — that fuel imprudent prescribing.
Teh pattern worsens when broad-spectrum agents are preferred over targeted therapy, or when antibiotics are available without oversight. Poor dosing, incomplete adherence, and agricultural use create a feedback loop that makes resistance more widespread. Stewardship, better diagnostics, and public education are keys to reversing this trend and protecting effective drugs. Collective action prevents catastrophe.
Diagnostics and Surveillance: Spotting Resistant Infections Early

A clinician watches a patient worsen despite standard therapy, then orders cultures and targeted susceptibility tests; that moment transforms suspicion into evidence and starts an investigative thread and containment.
Rapid molecular assays, point-of-care PCR and sequencing can reveal mutations conferring bactrim resistance within hours, guiding therapy and informing whether broader surveillance is neccessary to curb spread across facilities.
Public health labs collate isolates, map resistance hotspots and feed alerts to clinicians; linking local trends with national databases turns isolated failures into timely public health action and clinicians.
Timely reporting, interoperable data systems and clinician awareness shorten the lag between detection and response; investing in diagnostics is an investment in preserving effective antibiotics for tommorow's patients.
Stewardship Strategies Clinicians Can Implement Today Effectively
Clinicians can curb resistance by weaving evidence into daily practice: narrow-spectrum choices guided by culture data, delayed prescriptions when appropriate, and clear stop dates reduce selection pressure. Shared decision-making transforms a single prescription into a teachable moment—explain why bactrim may not be needed, discuss side effects, and set realistic recovery expectations. Rapid point-of-care tests and antibiograms should shape empiric therapy, shortening time to targeted treatment and lowering unnecessary broad-agent exposure.
Practical stewardship tools are simple but powerful: order sets that default to recomend durations, audit-and-feedback loops, and peer comparison reports that highlight prescriber patterns. Education sessions tied to local resistance trends make guidance relevance palpable, while pharmacist-physician collaborations streamline dose optimization and IV-to-oral switches. These interventions are scalable across settings and can be implemented today with modest resources, improving patient outcomes and slowing resistance emergence with measurable impact within months.
Public Health Prevention: Community Actions to Protect Antibiotics
A neighborhood clinic once tracked rising urinary infections and mobilized residents to change behaviours. Simple steps—hand hygiene campaigns, vaccination drives where available, and public education about not demanding antibiotics—slowed transmission. These stories remind health planners that small, coordinated moves can shift community risk.
Surveillance networks help spot resistant strains early, allowing targeted outreach and stewardship. Labs reporting local resistance patterns gives clinicians actionable data and lets pharmacies adjust prescribing guides. Community leaders must support testing access and safe disposal programs to reduce environmental antibiotic pressure.
Schools and workplaces can role-model good prescribing norms, teach when antibiotics are useless, and promote safe water and waste practices to protect the enviroment and preserve Bactrim efficacy for generations. Trimethoprim (PubChem) PubMed: TMP-SMX resistance






Email Us
Fill out all the fields below and press submit, a rep will contact you as soon as possible.