| Royal City Drugs |
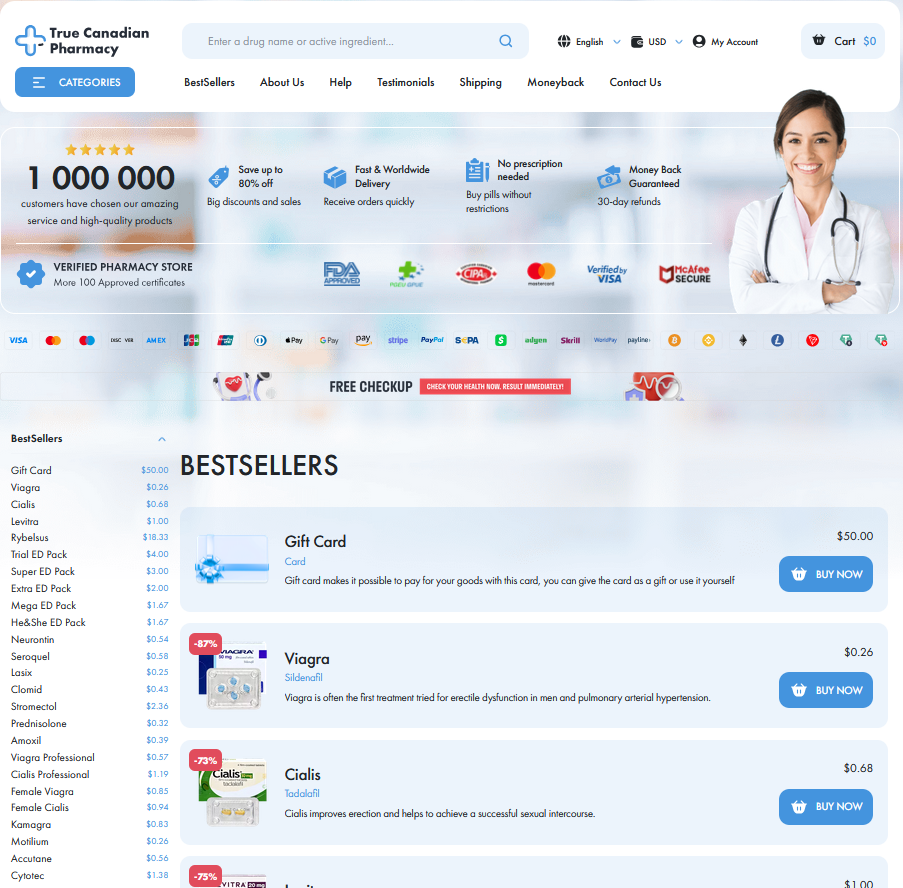
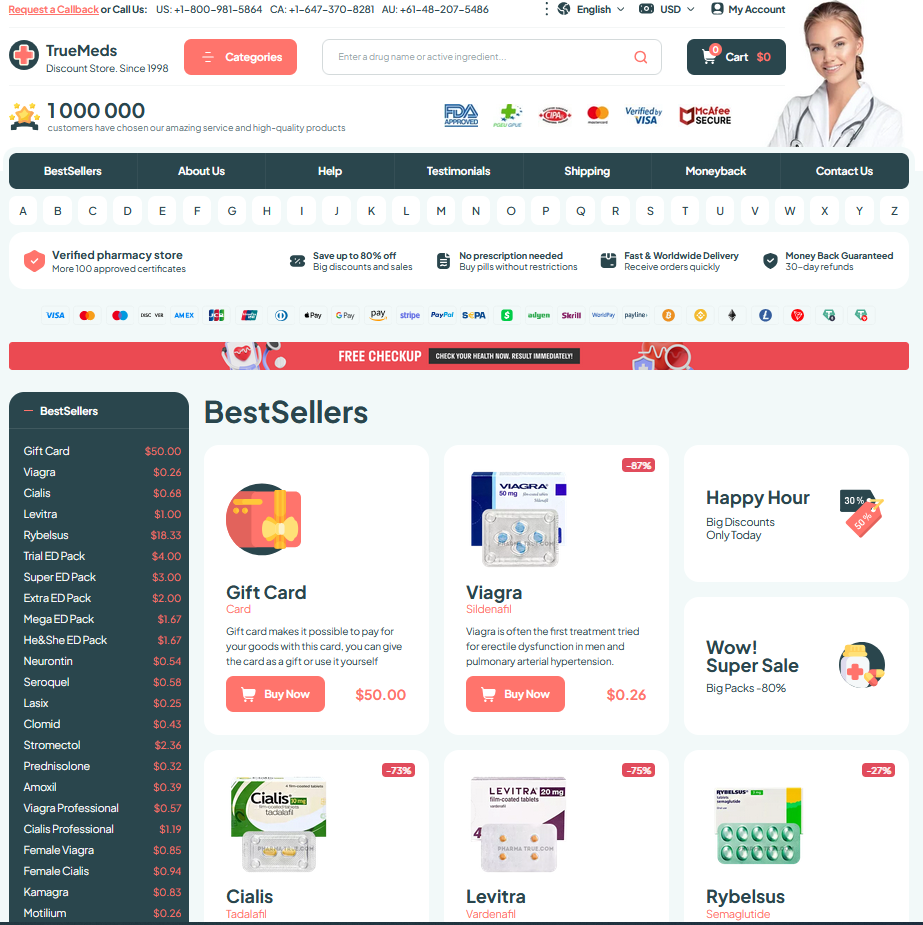
To Visit Online Pharmacy Click HERE ↓
Off-label Clonidine Uses: Insomnia, Anxiety, and More
How Clonidine Works: Mechanisms Behind Off-label Benefits
On a restless night, clonidine quietly dampens the brain’s alarm system by stimulating central α2‑adrenergic receptors, reducing norepinephrine release from the locus coeruleus. This lowers sympathetic tone, slows heart rate and blood pressure, and promotes sedation — a pharmacologic nudge toward calmer sleep and reduced hyperarousal.
At the synaptic level it exerts presynaptic inhibition, altering sleep architecture and attenuating noradrenergic arousal that fuels anxiety. Clinically, this produces calming effects Teh clinician can exploit for off‑label indications, especially when hyperadrenergic enviroment contributes to insomnia or sympathetic symptoms and improves stress responsivity.
Clonidine for Insomnia: Evidence, Dosing, Side Effects

I’ve seen patients trade nightlong anxiety for softer sleep when clonidine calms their hyperarousal; small trials and case series suggest modest improvements in sleep onset and REM suppression.
Typical adult dosing ranges from 0.05–0.2 mg at bedtime, starting low and titrating slowly; for children doses are lower and monitoring is essential. Teh evidence is limited and heterogenous, so clinicians often weigh benefits against risks.
Common adverse effects are sedation, dry mouth, dizziness and bradycardia; rebound hypertension can occur with abrupt stop, so gradual tapering is recomend. and routine blood-pressure monitoring.
Managing Anxiety Symptoms with Clonidine: Research Overview
I met a patient whose racing heart and sleepless nights persisted despite therapy; adding clonidine calmed the autonomic storm within days. The narrative isn’t universal, but it illustrates how alpha-2 agonism can reduce sympathetic arousal and interrupt the cascade of physical symptoms that often amplify worry and panic.
Clinical data are modest: small randomized trials and case series show benefit for hyperarousal, performance anxiety, and situational panic, but effect sizes vary. Many studies are heterogeneous in dosing and populations, and comparator arms often lack active control. Meta-analyses call for larger RCTs to clarify efficacy and optimal patient selection.
In practice, start low and titrate slowly while monitoring blood pressure and sedation. Recieve informed consent about rebound hypertension with abrupt cessation. For resistant symptoms consider adjunctive use with psychotherapy or SSRI, but clinicians should weigh limited evidence and tolerability before adoption.
Less Known Uses: Adhd, Opioid Withdrawal, Nightmares

In restless children and adults with ADHD, clonidine can temper hyperactivity and impulsivity by damping sympathetic tone and improving sleep, offering a useful adjunct when stimulants are ineffective. Occassionally too.
During opioid withdrawal clonidine blunts noradrenergic surges, reducing sweating, tremor, and anxiety so patients tolerate the process with less distress; Aparent benefits appear early but careful monitoring is often essential.
A clinical vignette shows a veteran regaining restful nights: low-dose clonidine calmed nocturnal agitation and nightmares, restoring daytime focus. Dose-related hypotension risk requires gradual titration and outpatient follow-up for safety.
Safety, Interactions, and Monitoring When Prescribing Clonidine
When I first considered clonidine for a restless patient, I worried about blood pressure drops; explaining bradycardia and rebound hypertension made informed consent concrete and human.
Baseline vitals, orthostatic checks, and medication reconciliation uncover risks like interactions with antihypertensives or sedatives; teh conversation also includes renal and hepatic function.
Start low and titrate slowly—children and elderly need smaller steps. Watch for somnolence, dry mouth, and rare severe hypotension; pulse and BP logs help track trends.
Coordinate with other prescribers, adjust doses if withdrawal is planned, and schedule follow-up within weeks. If adverse effects occured, hold dose and reassess; safety is collaborative. Document discussions and provide written instructions about missed doses, tapering, and emergency contacts immediately.
Practical Tips: Patient Selection, Tapering, Real-world Considerations
Start by choosing patients with clear target symptoms and stable cardiovascular status; avoid use in severe hypotension, bradycardia, or pregnancy unless specialist input. Screen for interacting meds and counsel on sedation risk; prefer lower starting doses for elderly and children. Occassionally consider comorbid ADHD or withdrawal contexts when benefits outweigh risks.
When stopping, taper slowly to prevent rebound hypertension and worsening sleep or anxiety—common after abrupt cessation. A practical schedule reduces dose by 10–25% every three to seven days, individualized by response; longer tapers may be neccessary after months of treatment. Monitor vitals and symptoms during reduction.
Start low, titrate, document consent; follow-up soon and ensure blood pressure monitoring for guidance. FDA label StatPearls review






Email Us
Fill out all the fields below and press submit, a rep will contact you as soon as possible.