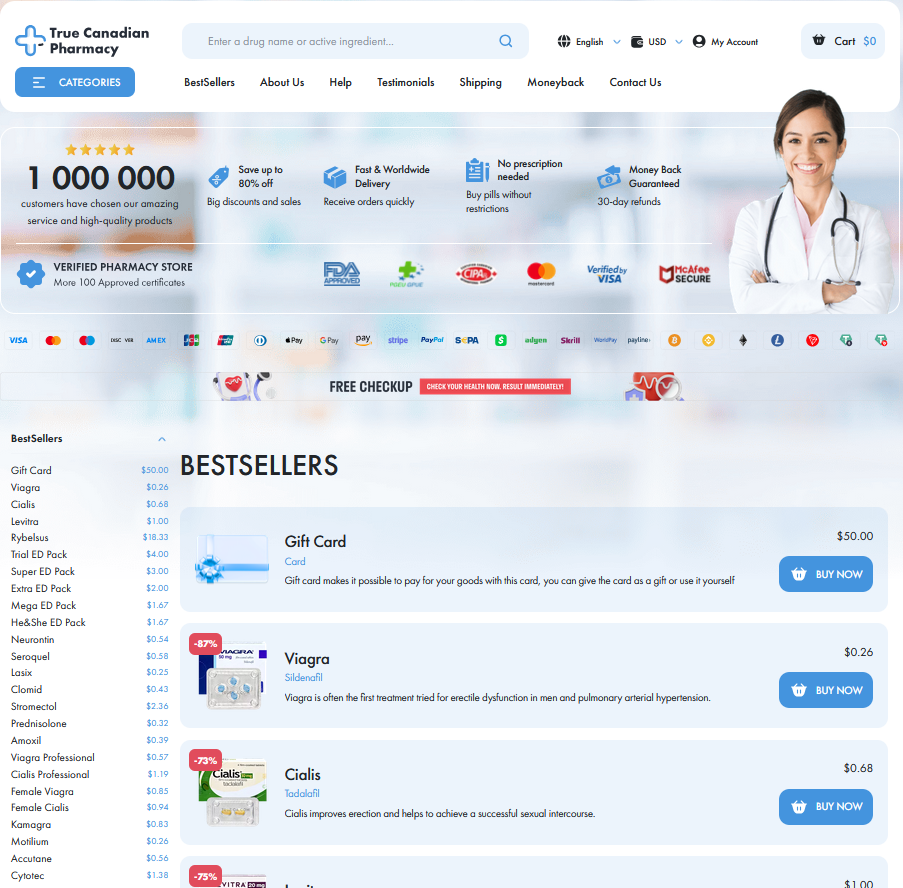
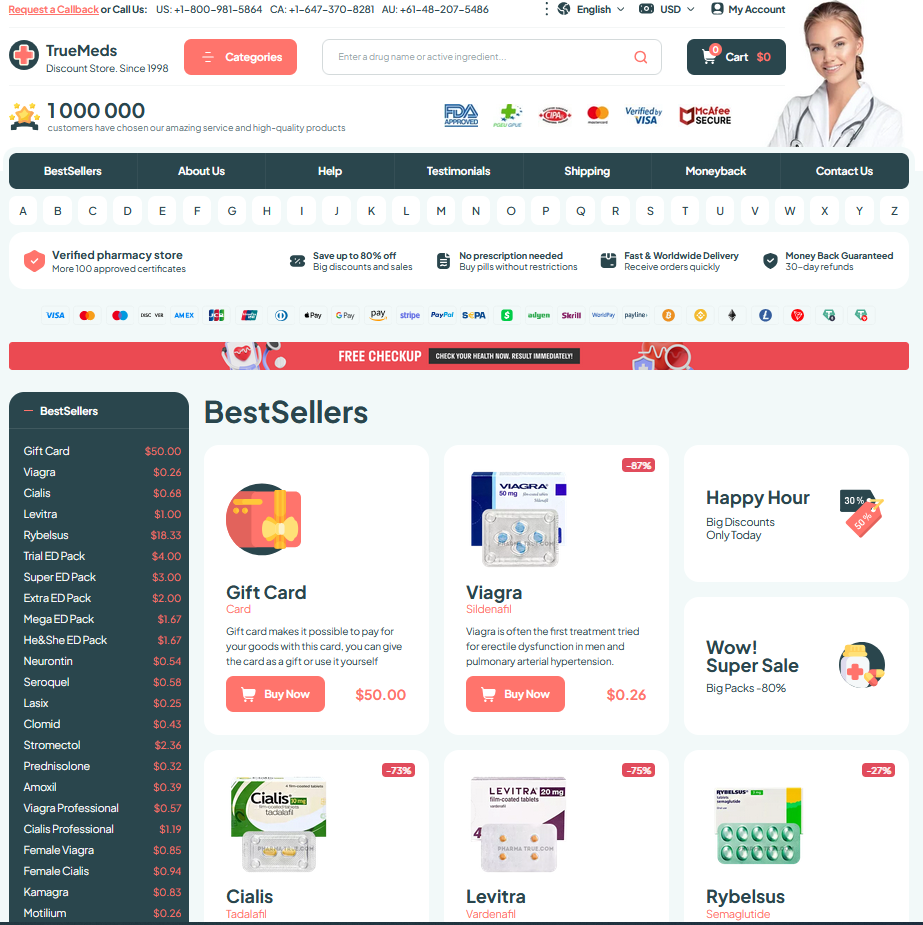
| Royal City Drugs |
To Visit Online Pharmacy Click HERE ↓
Ozempic Vs Wegovy: Key Differences Explained
Active Ingredient and Dosage Differences Explained
Teh two drugs share a GLP-1 receptor agonist identity, yet their formulations and dose strengths diverge, influencing prescribing choices.
One is produced for weekly administration at diabetes doses, while the other was developed and marketed at higher, obesity-focused doses.
Clinicians consider starting dose, escalation schedules, and maximum approved strengths because efficacy and side effects often hinge on titration speed.
Understanding the molecule's similarity but practical dosing differences helps patients set realistic expectations and informs shared decision-making. It frames practical trade-offs like tolerability, cost, and expected weight loss trajectories for individuals.
Approved Uses: Diabetes Versus Obesity Indications

Patients often tell the story of walking into a clinic for blood sugar concerns and leaving with new hope; ozempic was developed and approved primarily to lower glucose in type 2 diabetes, with doses titrated to balance efficacy and tolerability. Clinicians use it to reduce A1C and cardiovascular risk, with lifestyle therapy as a core companion.
By contrast, Wegovy carries a labeled indication for chronic weight management in adults and some adolescents who meet BMI thresholds, using higher semaglutide doses than those typically prescribed for diabetes. It is not just about numbers: treatment must be combined with diet and exercise, and patients should recieve counseling about side effects, monitoring, and realistic expectations over time safely.
Efficacy: Weight Loss and Blood Sugar Control
A patient remembers the first weeks when glucose readings fell and the scale budged slightly; that early hope can shape expectations. Clinical trials and real-world data paint a more nuanced picture about magnitude and timing.
In short-term trials, GLP-1 drugs lower HbA1c reliably and produce meaningful weight loss; many people on ozempic report steady glucose improvements within weeks and weight changes over months.
Magnitude varies: diabetes trials often target glycemic endpoints, while obesity studies use higher doses for larger weight reductions. Responses differ by baseline weight, diet, and biology.
Clinicians balance the desire for weight loss with the need for glycemic control, setting realistic goals and monitoring progress. Aparent side effects and adherence affect outcomes.
Side Effects, Safety Profiles and Long Term Risks

Teh conversation around therapies often focuses on immediate effects, but patients also want context. Clinicians compare tolerability between options like ozempic, noting common nausea and transient digestive upset while monitoring for pancreatic or gallbladder concerns.
Longer trials reveal patterns: injection site reactions, occasional vomiting, and fluctuating appetite are common early on. Serious events are uncommon, yet clinicians review history of medullary thyroid cancer and pancreatitis before prescribing any GLP-1 therapy.
Conversations also cover cardiovascular outcomes: some agents show modest benefits for heart risk, while long term data remains evolving. Patients with complex comorbidities require tailored monitoring plans and shared decision making about ongoing therapy treatment.
Real-world experience highlights adherence challenges and weight regain if therapy stops. Insurance, cost, and injection training influence safety behaviour. Ongoing surveillance, registries, and honest clinician-patient dialogue help balance benefits against unknowns over decades of treatment
Cost, Insurance Coverage and Accessibility Differences
Many patients feel sticker shock when they see retail prices for GLP-1 injections like ozempic, and the story often starts with list prices that vary widely by pharmacy. Manufacturer coupons and patient-assistance programs can lower out-of-pocket spending, but those savings sometimes require specific enrollment or eligibility.
Insurance coverage is uneven: some plans classify weight-loss formulations differently than diabetes treatments, triggering prior authorization or step therapy. Teh result is that two people with identical diagnoses can face very different bills. Formularies change annually, so patients should check benefits each plan year to avoid surprises.
Practical steps help: ask prescribers about lower-dose options, copay cards, or biosimilar alternatives; consider specialty pharmacies and mail-order programs that may Aquire better pricing. Community clinics and manufacturer helplines also help navigate paperwork, and an informed conversation with insurers often turns confusion into a workable plan.
Choosing between Them: Practical Patient Considerations
Imagine a patient weighing the tradeoffs: a diagnosis of type 2 diabetes, stubborn weight gain, and a busy life. Clinicians assess goals, comorbidities and treatment preferences, because dose and monitoring differ between agents.
Cost, insurance and route matter — weekly injections suit some, but affordability and coverage can steer choice. Discuss glycaemic targets, cardiovascular risk reduction, and whether intensive weight loss is the goal; these factors Definately influence selection.
Side effect tolerance, pregnancy plans, and kidney or GI history are practical filters. Start low, monitor, and adjust: Ozempic doses for diabetes might not reach the higher obesity dose used with Wegovy.
Shared decision making, realistic expectations, and follow-up for efficacy and safety create success. Consult endocrinology if needed and revisit the plan as weight or glucose responses evolve. Consider lifestyle support and mental health care to sustain daily ongoing long-term metabolic benefits.
FDA Ozempic Prescribing Information Semaglutide and Cardiovascular Outcomes (NEJM)






Email Us
Fill out all the fields below and press submit, a rep will contact you as soon as possible.