| Royal City Drugs |
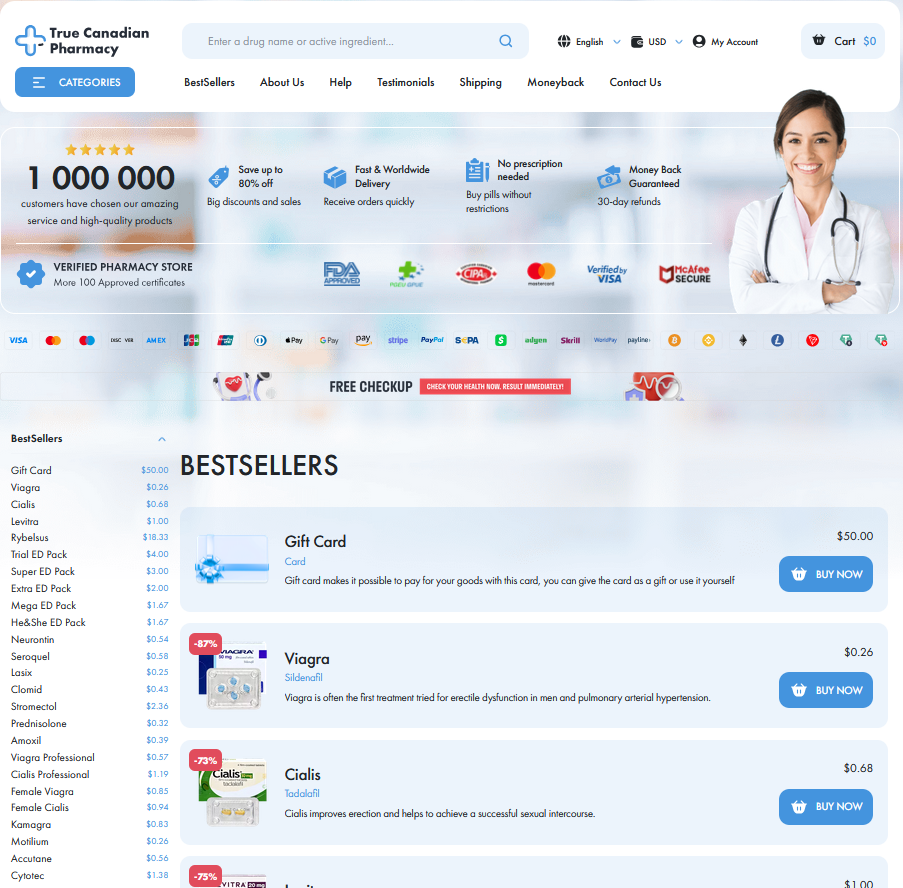
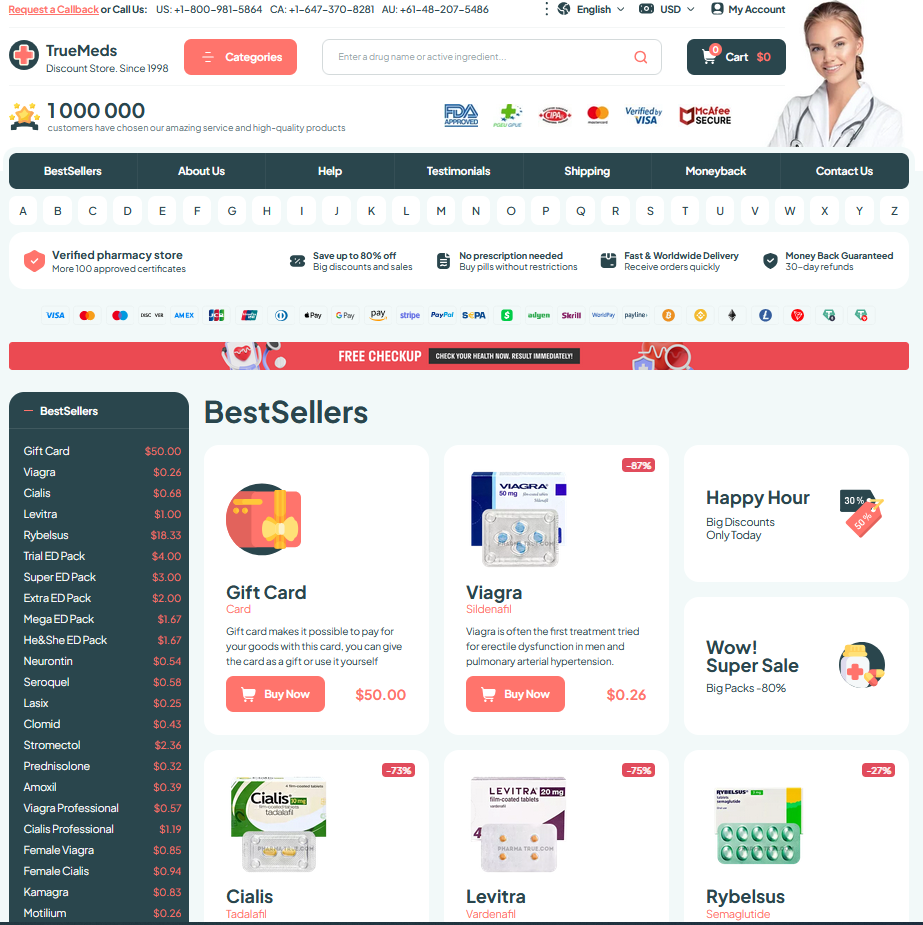
To Visit Online Pharmacy Click HERE ↓
Dosing Strattera: What to Know
Understanding Starting Doses and Titration Schedules
I remember discussing first dose decisions with a patient who worried about side effects. Clinicians usually start low, often 0.5 mg/kg for children or about 40 mg for adults, to let the body adjust.
Titration is gradual: after a few days to weeks the dose is raised toward a maintenance level, commonly near 1.2 mg/kg or around 80 mg daily, with typical maximums near 100 mg. Monitoring for response and heart rate, blood pressure, and mood is key.
Expect gradual adjustments; Teh clinician tailors increases to maximize benefit and safety.
Weight-based Dosing: Children Versus Adult Considerations

Kids and adults metabolize medication differently, so dosing often follows weight-based calculations and careful titration. Clinicians start cautiously, watching growth and comorbidities while adjusting for tolerance and efficacy over time.
Families recieve clear plans: children’s doses are usually mg/kg, adults use fixed doses. With strattera, expect slower titration and regular check-ins to monitor heart rate and mood, sleep and appetite.
Dose changes hinge on benefits versus side effects; smaller, frequent adjustments accommodate developmental shifts. Open dialogue with prescribers ensures safety, and vitals checks provide objective feedback over months and follow-up.
Adjusting Dose for Effectiveness and Side Effects
Starting a medication often feels like stepping onto unfamiliar ground; I remember a patient hesitating at the first dose, hopeful but cautious. With strattera, dose changes are a dialogue between you and your clinician, guided by symptoms, not a fixed timetable.
Titration usually moves slowly. Small increases every few weeks let clinicians spot benefits and bother. Keep a simple symptom log: mood, focus, sleep, and note any physical reactions. Blood pressure and heart rate checks can be useful early on.
Side effects can fade as the brain adjusts, but some warrant a pause or reduction. Headache, stomach upset, or sleep changes are common and often brief; Occassionally, more serious signs like chest pain demand immediate attention. Trust your instinct and report what you observe.
Work closely with your prescriber, document changes, and prioritize the lowest effective dose for safer results.
When to Expect Improvements and Timeline

You might remember the first week when the medication felt like a quiet background change; with strattera improvements are gradual, not overnight. Many notice subtle focus gains and calmer thinking before clearer behavioral change.
Timelines vary: some children begin to improve in two to four weeks, while full effects often take six to twelve. Adults may see earlier cognitive changes but also need weeks for mood and routine shifts.
If after eight to twelve weeks there’s limited improvement, clinicians occassionally adjust dose or revisit diagnosis. Keep a simple symptom log to make trends clear and decisions easier.
Be patient; expect incremental gains and realistic timelines, check in often so prescribers guide dose changes with evidence.
Managing Common Side Effects and Safety Tips
I remember a patient describing mornings when nausea and dry mouth made coffee less comforting; with strattera these effects often fade as the body adjusts. Start slowly, take medication with food, and expect appetite suppression, sleep changes, or dizziness — Teh key is tracking symptoms and keeping a simple log so you and your clinician can weigh benefits against tolerability.
Safety means watching for mood shifts or suicidal thoughts, checking blood pressure and heart rate before changes, and avoiding interacting drugs like MAOIs or certain antihistamines. Report severe reactions (chest pain, priapism) immediately, and don’t stop abruptly; dose adjustments are best guided by your prescriber. Occassionally labs or ECGs are ordered for higher-risk patients, and regular follow-up ensures the regimen is both effective and safe. Keep open communication, document side effects, and carry a list of medications to every appointment.
Switching, Stopping, and Drug Interactions Explained
When shifting from a stimulant, many clinicians halt the prior med before initiating atomoxetine; history of mood disorders and suicide risk shape the plan. Definately discuss timing with your prescriber.
Stopping abruptly can cause return of symptoms rather than withdrawal; a monitored taper may be used if adverse effects occur. Track mood, sleep, and appetite during the transition.
Major interactions include MAOIs and strong CYP2D6 inhibitors; herbal supplements and cold meds matter too. Always list prescription and OTC drugs, so clinicians can prevent serious cardiovascular or serotonin problems during changes. MedlinePlus - atomoxetine DailyMed - atomoxetine label






Email Us
Fill out all the fields below and press submit, a rep will contact you as soon as possible.